The diagnosis of prostatitis includes more than 5 mandatory and 4 additional procedures. A single rectal exam or ultrasound of the prostate gland cannot tell for sure whether men have prostatitis. This is because many urological diseases have a similar clinical picture, and only a comprehensive differential examination excludes the possibility of misdiagnosis.

How to pass the inspection
Men are recommended to undergo a preventive examination of the prostate by a urologist 1-2 times a year (prostatitis, adenoma and other pathologies of the prostate are asymptomatic in the first stage). If signs of the disease appear, contact a specialist immediately. Such symptoms include pain in the lower abdomen and groin, difficulty urinating and erection.
The doctor begins by collecting the patient's complaints and history, and then performs a general examination. The next step in suspected prostatitis is a rectal examination (palpation of the prostate through the man's rectum). Finger research allows the doctor to evaluate the following parameters:
- Prostate size.
- Surface (smooth or bumpy).
- Density of the gland (soft or stony).
- The presence or smoothness of the central groove.
- The man's sensitivity when examining the prostate (do they feel pain).

Analyzes
If the rectal examination and medical history indicate prostatitis, the urologist's next step is to refer the patient for laboratory tests. According to clinical standards, the following types of tests are mandatory:
- clinical analysis of urine;
- general blood test;
- urine sowing for flora;
- when an infection is detected, the sensitivity of pathogens to antibiotics is determined.

A complete blood count helps to confirm acute prostatitis - with this diagnosis, the number of neutrophils increases, the leukocyte formula shifts to the left and the level of eosinophils drops sharply. An increase in ESR is also possible. Chronic inflammation is characterized by a low hemoglobin content (below 100 grams/liter of blood).
In order to rule out prostate cancer, a blood serum test is performed for the content of PSA - a prostate-specific antigen. Its increased amount indicates the presence of tumors, but does not determine their nature (benign or malignant). To find out this parameter, a biopsy of the prostate is performed with a histological examination of the obtained material.
prostate secret
During the rectal examination of the prostate, the urologist pays attention to the selected discharge. It is usually thick, odorless, and white in color. The maximum amount is 1-2 drops (3-5 ml). It should not contain pus or blood contamination, as this is a sign of disease. The consistency of the juice plays a role - if it comes out in clots, the man has diverticular prostatitis. A more detailed study of the material enables laboratory research.
Microscopic and bacteriological examination of prostate secretion is based on the number of leukocytes, lecithin particles, amyloid bodies, macrophages, pathogenic and opportunistic organisms. Prostatitis is characterized by the following differences:
- Acute prostatitis: the color of the secretion is yellowish, the smell is sweet, the pH value is acidic, less than half of the leukocytes and no more than ¼ of the epithelial cells are found.
- Chronic bacterial prostatitis: yellow or brown color, sour smell, acidic pH, less than half of leukocytes, macrophages (over 15 years), many amyloid bodies.
- Chronic non-bacterial prostatitis: reddish, brown in color, odorless, leukocytes are normal, macrophages (10-20) can be seen, many amyloid bodies are present.

In some cases, the study of the secret does not allow detecting prostatitis due to incorrect indicators. Unclear data will be in the presence of inflammation of other organs, in case of a body temperature above 39 degrees. Material sampling is not possible with rectal massage contraindications (extraction of prostate juice using this method): hemorrhoids, rectal fissures, with exacerbation of prostate tuberculosis.
Urine
General and cytological analysis of urine does not require special preparation. The man should collect the material in a container in the morning, before breakfast (it is better to buy a sterile plastic container at the pharmacy). A few hours before this, the patient is not recommended to empty the bladder, and he should not take medicine or alcoholic beverages a day before.
In the catarrhal form of the disease, no deviations from the norm can be observed during the general analysis of urine. In the case of late-stage prostatitis, purulent fibers are detected in the examined material, which precipitate.

Examining a man's urine makes it possible to diagnose leukocyturia (an increase in the level of leukocytes, which occurs in the case of inflammation). A urine culture is performed to determine the type of pathogens. Signs of pathogens appear in the urine in case of infectious prostatitis or complications such as cystitis and urethritis or pyelonephritis.
swabs from the urethra
A urethral smear is a form of examination that confirms inflammation caused by pathogens such as Trichomonas, gonococci, Candida. It is prescribed for chronic pelvic pain syndrome, itching in the groin, rash on the penis, difficulty urinating. The study of the removed material allows for differential diagnosis - distinguishing prostatitis, urethritis or sexually transmitted diseases, which often have similar symptoms or occur simultaneously.
The disease is diagnosed only on the basis of a properly collected smear. The man must abstain from sex for 2 days before taking the substance. One hour before the procedure, do not go to the toilet a little. If the patient is taking NSAIDs or antibiotics, then this analysis is useless - the data is incorrect.
Spermogram
Spermogram - analysis of male ejaculation. In addition to prostatitis, diseases of the seminal vesicles and testicles are diagnosed in this way, and infertility can be detected. The material submitted by a man with a body temperature not higher than 39 degrees, not taking antibiotics and staying for 2-3 days is correct. Prostate massage is not recommended one day before sperm donation.
The spermogram contains three types of tests. Macroscopic analysis includes the study of sperm volume, color, viscosity and liquefaction time. Microscopic examination reveals the quantity and quality of sperm. The biochemical analysis determines the concentration of fructose, zinc, alpha-glucosidase, L-carnitine in the ejaculate. In case of bacterial prostatitis, anti-sperm antibodies can be detected.
In the case of prostatitis, the spermogram can reveal many abnormalities. For example, reduced sperm volume (less than 1. 5 ml), low sperm concentration in 1 ml (less than 15 million), asthenozoospermia (more than 40% of immotile sperm), akinospermia (more than 32% of immotile sperm) ).
Prostate tissue
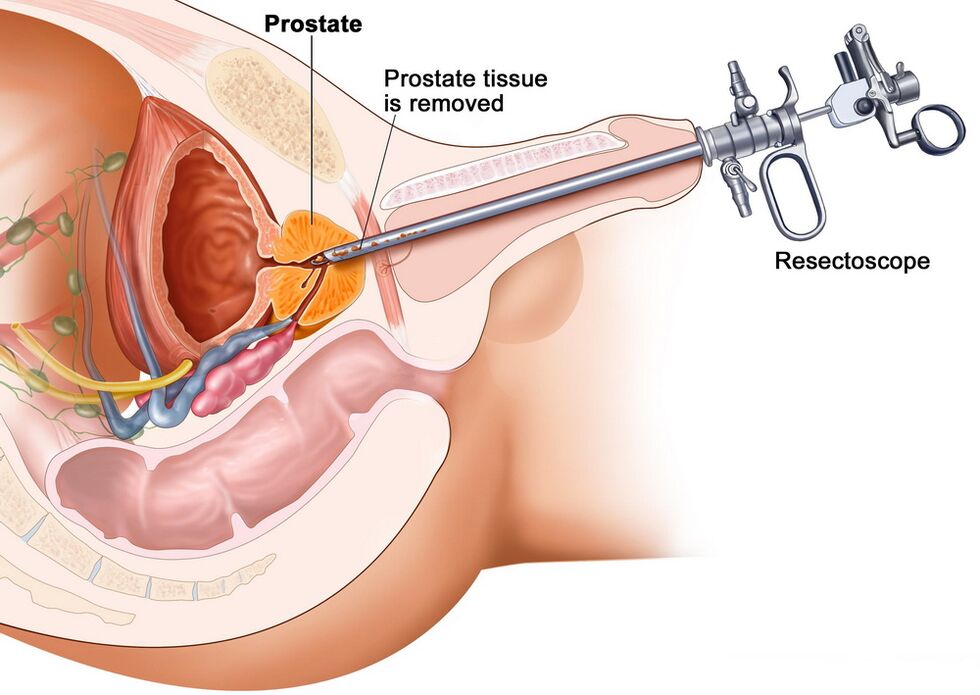
When examining an enlarged prostate, it is not always possible to understand the nature of seals and appendages with the help of rectal examination, urine and blood tests. It can be a benign pathology (adenoma, prostatitis) or malignant (cancer). An accurate diagnosis is helped by the microscopic examination of the tissues of the prostate, which are obtained by biopsy.
The procedure is as follows: the patient is transrectally inserted with an ultrasonic machine sensor, at the end of which there is a gun with a biopsy needle. With a sharp tip, a microscopic part of the glandular tissue is cut off and sent to the laboratory for examination. The test is carried out using the method of comparing the parameters of the material with the standards of the Gleason table.
In the case of congestive, viral or bacterial prostatitis, the size of the gland cells is reduced, and the amount of connective tissue in the intercellular space increases. Atypical cells with altered nuclei are not observed. When a man has prostate cancer, the gland cells become large and cluster together, revealing abnormal changes.
Ultrasound, MRI and other methods
Instrumental tests are performed to confirm the diagnosis and to determine the characteristics of the developmental stage and course of the disease. In the case of pathologies of the pelvic organs, the following examination methods are used:
- conventional ultrasound;
- transrectal ultrasound;
- magnetic resonance imaging (MRI);
- CT scan.
These methods allow you to find out the shape, thickness, width, length, mass, structural uniformity, echogenicity, vascularization (vascular pattern) of the prostate. These parameters are necessary to determine urological pathologies: ultrasound, CT and MRI show inflammatory, proliferative and oncological diseases of the prostate.
Classic ultrasound has the greatest inaccuracy, but this method is still used because it is easy to use and affordable. Transrectal ultrasound is considered the "gold standard" for detecting prostatitis, but prostate cancer is difficult to see this way (especially in the early stages). MRI and CT are the most accurate in determining tumors, but they are complex and expensive procedures, so they are performed whenif other research methods most likely show oncology.
Home inspection
The prostate can be examined at home and the primary symptoms of urological pathologies can be identified. Of course, this will not be a diagnosis of chronic prostatitis, since the cause of the enlarged gland cannot be reliably determined. But the presence of warning signs during an independent examination of the body is a significant reason for an immediate visit to the urologist.
Just like that, without self-diagnosis, it's not worth it. Indications for home testing include:
- Impaired urodynamics (frequent urge to urinate).
- Weak stream, inability to empty the bladder completely.
- Unpleasant feeling in the abdomen or groin (for example, painful urination).
- Decreased sexual desire, weakening of erection.
- Purulent impurities or the discoloration of urine to white or brown.
- Spermatorrhoea or prostorrhoea (discharge from the penis).
At home, the examination is carried out according to the same scheme as in the doctor's office. First, a man needs to clean his intestines - within 10-12 hours, he needs to do an enema or take a laxative. Take a bath immediately before the procedure. Next, lie on your side, bend your knees, insert your index finger into the rectum (first put it on the tip of your finger and smear the top with Vaseline).
A digital rectal examination is performed by palpating the posterior wall of the intestine and detecting the adjacent prostate. The gland is easy to recognize - it feels like a small nut to the touch. Bad symptoms: prostate enlargement, non-circular shape, presence of tubercles, pain on palpation.These signs indicate inflammation of the prostate or other pathological processes. When identifying them, you should definitely consult a urologist, because a more accurate diagnosis and treatment plan is required.
























